Learn more about glaucoma
What is glaucoma? Symptoms, treatment options and more!
At a Glance:
Things to know and remember:
- Glaucoma is a group of eye diseases that can cause vision loss and blindness by damaging a nerve in the back of your eye called the optic nerve.
- Glaucoma is a leading cause of vision loss and blindness in the United States — especially for older adults and African Americans.
- Symptoms may start so slowly that you may not notice them.
- The only way to find out if you have glaucoma is to get a comprehensive dilated eye exam.
- There are several types of treatment for glaucoma, including medicines (usually eye drops), laser treatment, and surgery
- There’s no cure for glaucoma, but early treatment can often stop the damage and protect your vision.
About Glaucoma
What is a glaucoma?
Glaucoma is commonly referred to as the silent thief of sight and is one of the leading causes of preventable blindness worldwide. It affects over 3 million Americans and 70 million people around the world, most of whom don’t even know they have it.
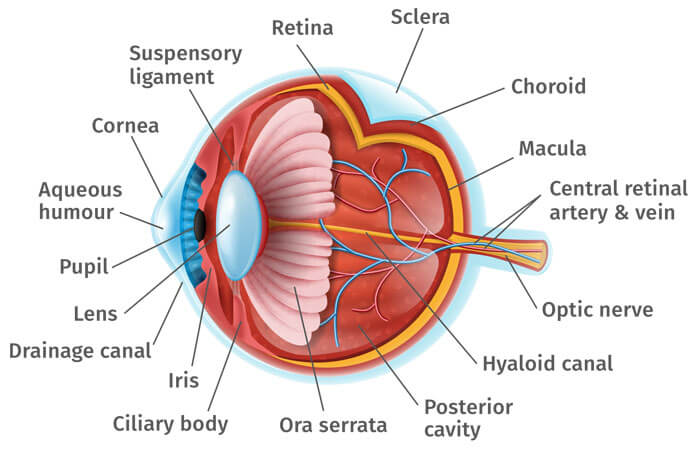
Glaucoma is a group of eye diseases characterized by damage to the optic nerve, the nerve that transmits visual information from the eye to the brain. In most cases, this nerve damage is produced by increased fluid pressure within the eye. This elevated pressure is caused by a backup of fluid in the eye. Over time, it causes damage to the optic nerve. Through early detection, diagnosis and treatment, you and your doctor can help to preserve your vision and often protect your eyes against serious vision loss.
Think of your eye as a sink, in which the faucet is always running and the drain is always open. The aqueous humor is constantly circulating through the anterior chamber. It is produced by a tiny gland, called the ciliary body, situated behind the iris. It flows between the iris and the lens and, after nourishing the cornea and lens, flows out through a very tiny spongy tissue, only one-fiftieth of an inch wide, called the trabecular meshwork, which serves as the drain of the eye. The trabecular meshwork is situated in the angle where the iris and cornea meet. When this drain becomes clogged, aqueous cannot leave the eye as fast as it is produced, causing the fluid to back up. But since the eye is a closed compartment, your `sink´ doesn´t overflow; instead the backed up fluid causes increased pressure to build up within the eye. We call this open (wide) angle glaucoma.
To understand how this increased pressure affects the eye, also think of your eye as a balloon. When too much air is blown into the balloon, the pressure builds, causing it to pop. But the eye is too strong to pop. Instead, it gives at the weakest point, which is the site in the sclera at which the optic nerve leaves the eye.
The optic nerve is part of the central nervous system and carries visual information from the eye to the brain. This cranial nerve is made up of over one million nerve axons, which are nerve fiber extensions of the retinal ganglion cells. When the eye pressure is increased and/or other inciting factors exist, the optic nerve becomes damaged and the retinal ganglion cells undergo a slow process of cell death termed “apoptosis.” The death of the retinal cells and degeneration of the nerve fibers results in permanent vision loss. Early diagnosis and treatment of glaucoma can help prevent blindness.
Diagnosis
How glaucoma detected?
Glaucoma is detected through a comprehensive eye exam and a series of tests that include:
- Visual acuity test: This eye chart test measures how well you see at various distances. It’s the same basic vision test with which we all are familiar.
- Dilated eye exam: Drops are placed in your eyes to widen, or dilate, the pupils. We then use a special magnifying lens to examine your optic nerve and retina for signs of damage and other eye problems. Most people have had a dilated eye exam at some point in their lives.
- Visual field test: This test measures your peripheral vision. Visual field is an important measure of the extent of damage to your optic nerve from elevated IOP. In glaucoma, it is the peripheral (side) vision that is most commonly affected first. Testing your visual field lets your doctor know if peripheral vision is being lost. There are several methods of examination available to your doctor; visual field testing has advanced significantly in recent years. In computerized visual field testing you will be asked to place your chin on a stand, which appears before a concave computerized screen. Whenever you see a flash of light appear, you press a buzzer. At the end of this test, your doctor will receive a printout of your field of vision. New software has been developed to help your doctor analyze these tests as well as monitor progression of visual field loss over successive tests
- Tonometry: An instrument that measures the pressure inside the eye. Numbing drops are instilled in your eye for this test. Your doctor places a numbing eye drop in your eye. Then you sit at a slit-lamp, resting your chin and forehead on a support that keeps your head steady. The lamp, which lets your doctor see a magnified view of your eye, is moved forward until the tonometer, a plastic prism, barely touches the cornea to measure your IOP. The test is quick, easy and painless.
- Pachymetry: A numbing drop is instilled in your eye. We then use an ultrasonic wave instrument to measure the thickness of your cornea. Central corneal thickness (CCT) is an important measure and helps your doctor interpret your Intra Ocular Pressure (IOP) levels. Some people with thin central corneal thickness will have pressures that are actually higher than when measured by tonometry. Likewise, those with thick CCT will have a true IOP that is lower than that measured. Measuring your central corneal thickness is also important since recent studies have found that thin CCT is a strong predictor of developing glaucoma in patients with high IOP.
- Ophthalmoscopy: Using an instrument called an ophthalmoscope, your eye doctor can look directly through the pupil at the optic nerve. Its color and appearance can indicate whether or not damage from glaucoma is present and how extensive it is. This technique remains the most important in diagnosing and monitoring glaucoma.
- Gonioscopy: Your doctor may perform gonioscopy to closely examine the trabecular meshwork and the angle where fluid drains out of the eye. After numbing the eye with anesthetic drops, the doctor places a special type of hand-held contact lens, with mirrors inside, on the eye. The mirrors enable the doctor to view the interior of the eye from different directions. In this procedure, the doctor can determine whether the angle is open or narrow. Individuals with narrow angles have an increased risk for a sudden closure of the angle, which can cause an acute glaucoma attack. Gonioscopy can also determine if anything, such as abnormal blood vessels or excessive pigment, might be blocking the drainage of the aqueous humor out of the eye.
- Imaging: Photographs and computerized imaging of the optic nerves help detect damage from glaucoma. These tests are periodically repeated in patients with glaucoma to detect progression of the disease. A number of new and highly sophisticated image analysis systems are now available to evaluate the optic nerve and retinal nerve fiber layer, the areas of the eye damaged by glaucoma. These devices include scanning laser tomography (e.g. HRT3), laser polarimetry (e.g. GDX), and ocular coherence tomography (e.g. older time-domain OCT or newer spectral-domain OCT). These instruments can help your doctor by giving a quantitative measure of the anatomical structures in the eye. Photographs of the optic nerve can also be useful to follow the progression of damage over time. Large databases have been established to compare an individual’s anatomic structures to those of other patients in the same age group. This software and technology are developing rapidly and show great promise. However, they have not yet evolved to replace ophthalmoscopy, where the doctor looks directly at the optic nerve.
Treatment Options
Can glaucoma be cured?
No. There is no cure for glaucoma. Vision lost from the disease cannot be restored.
Glaucoma and Children
How is an eye examination given to an infant or young child?
If glaucoma is suspected in a child under the age of four, it is often necessary to perform an examination with the child under anesthesia. Under anesthesia, the doctor is best able to test the child’s intraocular pressure (tonometry) and evaluate the angles or dimensions of the eye (gonioscopy). Gonioscopy assists the doctor in determining whether the eye is functioning properly: producing, circulating, and draining the fluid or aqueous humor within the eye.
Does my insurance plan
cover my eye care?
Find out what insurance we accept and what is covered by insurance.
Learn more about our glaucoma specialists
Physician information including education, training, practice location and more.
Schedule an Appointment
Schedule an appointment with one of our specialists.





