Learn more about corneal eye care
What is corneal eye care? Symptoms, treatment options and more!
At a Glance:
Things to know and remember:
- The cornea is the clear “window” that allows light to pass into the eye.
- When the cornea is damaged, light rays entering the eye are scattered irregularly, decreasing one’s quality of vision.
- Corneal problems can be caused by injury, allergies or disease.
- There are a number of medical and surgical therapies to maintain or restore corneal clarity -- and your clarity of vision.
- The corneal specialists and surgeons at Eye Consultants of Pennsylvania are Board-Certified and Fellowship-trained. Quality and experience you can count on.
About The Cornea
What is cornea?
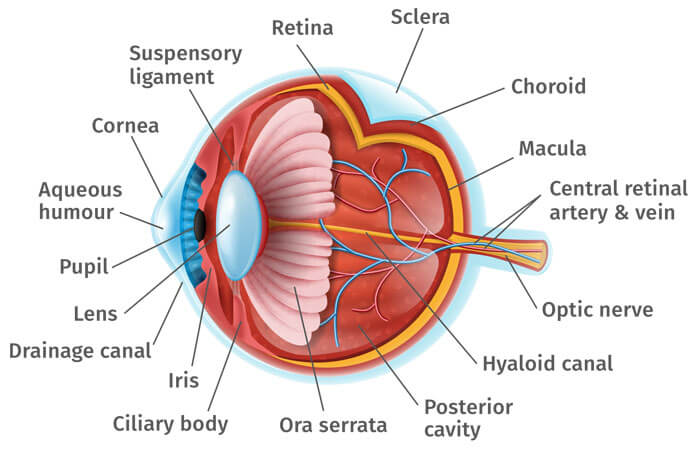
The cornea is the eye’s outermost layer. It is the clear, domeshaped surface that covers the front of the eye. It plays an important role in focusing your vision. Although the cornea may look clear and seem to lack substance, it is a highly organized tissue. Unlike most tissues in the body, the cornea contains no blood vessels to nourish or protect it against infection. Instead, the cornea receives its nourishment from tears and the aqueous humor (a fluid in the front part of the eye that lies behind the cornea). The tissues of the cornea are arranged in three basic layers, with two thinner layers, or membranes, between them. Each of these five layers has an important function, and each is subject to unique risks and diseases.
Although the cornea may look clear and seem to lack substance, it is a highly organized tissue. Unlike most tissues in the body, the cornea contains no blood vessels to nourish or protect it against infection. Instead, the cornea receives its nourishment from tears and the aqueous humor (a fluid in the front part of the eye that lies behind the cornea).
The tissues of the cornea are arranged in three basic layers, with two thinner layers, or membranes, between them. Each of these five layers has an important function. These layers are:
Epithelium: The epithelium is the cornea’s outermost layer. Its primary functions are to block the passage into the eye of foreign material, such as dust, water, and bacteria; and to provide a smooth surface to absorb oxygen and nutrients from tears, which are then distributed to the other layers of the cornea. The epithelium is filled with thousands of tiny nerve endings, which is why your eye may hurt when it is rubbed or scratched. The part of the epithelium that epithelial cells anchor and organize themselves to is called the basement membrane.
Bowman’s membrane: The next layer behind the basement membrane of the epithelium is a transparent film of tissue called Bowman’s layer, composed of protein fibers called collagen. If injured, Bowman’s layer can form a scar as it heals. If these scars are large and centrally located, they may cause vision loss.
Stroma: Behind Bowman’s layer is the stroma, which is the thickest layer of the cornea. It is composed primarily of water and collagen. Collagen gives the cornea its strength, elasticity, and form. The unique shape, arrangement, and spacing of collagen proteins are essential in producing the cornea’s light-conducting transparency.
Descemet's Membrane: Behind the stroma is Descemet’s membrane, a thin but strong film of tissue that serves as a protective barrier against infection and injuries. Descemet’s membrane is composed of collagen fibers that are different from those of the stroma, and are made by cells in the endothelial layer of the cornea. Descemet’s membrane repairs itself easily after injury.
Endothelium: The endothelium is the thin, innermost layer of the cornea. Endothelial cells are important in keeping the cornea clear. Normally, fluid leaks slowly from inside the eye into the stroma. The endothelium’s primary task is to pump this excess fluid out of the stroma. Without this pumping action, the stroma would swell with water and become thick and opaque. In a healthy eye, a perfect balance is maintained between the fluid moving into the cornea and the fluid pumping out of the cornea. Unlike the cells in Descemet’s membrane, endothelial cells that have been destroyed by disease or trauma are not repaired or replaced by the body.
The cornea is the clear “window” that allows light to pass into the eye. When the cornea is damaged, either by injury, allergies or disease, light rays entering the eye are scattered irregularly, decreasing one’s quality of vision.
The cornea acts as a barrier against dirt, germs, and other particles that can harm the eye. The cornea shares this protective task with the eyelids and eye sockets, tears, and the sclera (white part of the eye). The cornea also plays a key role in vision by helping focus the light that comes into the eye. The cornea is responsible for 65-75 percent of the eye’s total focusing power.
The cornea and lens of the eye are built to focus light on the retina, which is the light-sensitive tissue at the back of the eye. When light strikes the cornea, it bends—or refracts—the incoming light onto the lens. The lens refocuses that light onto the retina, which starts the translation of light into vision. The retina converts light into electrical impulses that travel through the optic nerve to the brain, which interprets them as images.
The refractive process the eye uses is similar to the way a camera takes a picture. The cornea and lens in the eye act as the camera lens. The retina is like the film (in older cameras), or the image sensor (in digital cameras). If the image is not focused properly, the retina makes a blurry image.
The cornea also serves as a filter that screens out damaging ultraviolet (UV) light from the sun. Without this protection, the lens and the retina would be exposed to injury from UV rays.
Every time we blink, tears are distributed across the cornea to keep the eye moist, help wounds heal, and protect against infection. Tears form in three layers:
An outer, oily (lipid) layer that keeps tears from evaporating too quickly and helps tears remain on the eye;
A middle (aqueous) layer that nourishes the cornea and the conjunctiva – the mucous membrane that covers the front of the eye and the inside of the eyelids;
A bottom (mucin) layer that helps spread the aqueous layer across the eye to ensure that the eye remains wet.
Cornea Conditions
What are some common conditions that affect the cornea?
The most common conditions involve injuries, allergies and disease. Treatment options depend upon the cause of the problem but can include options from contact lenses to laser surgery to corneal transplant. Based on your vision and examination, our corneal specialists will discuss with you the most appropriate treatment options.
If you have a corneal injury, an allergy affecting your cornea or a corneal disease or disorder, you could experience pain in the eye, a sensitivity to light, reduced vision or blurry vision, redness or inflammation in the eye, or headache, nausea or fatigue. Symptoms vary, both in their appearance and their severity.
The most common allergies that affect the eye are those related to pollen, particularly when the weather is warm and dry. Symptoms in the eye include redness, itching, tearing, burning, stinging, and watery discharge, although usually not severe enough to require medical attention. Antihistamine decongestant eyedrops effectively reduce these symptoms. Rain and cooler weather, which decreases the amount of pollen in the air, can also provide relief. For more information see Facts about Pink Eye (Conjunctivitis).
Contact Lens Related Infections are a common reason to consult a cornea specialist. Contact lens use (especially overnight wear) increases the risk of corneal infection. Corneal infections pose a serious threat to your vision and are treated aggressively with topical antibiotics. Patients no longer interested in wearing contact lenses may inquire about LASIK Laser Vision Correction.
Dry eye is a condition in which the eye produces fewer or lower quality tears and is unable to keep its surface lubricated. The main symptom of dry eye is usually a scratchy feeling or as if something is in your eye. Other symptoms include stinging or burning in the eye, episodes of excess tearing that follow periods of dryness, discharge from the eye, and pain and redness in the eye. Sometimes people with dry eye also feel as if their eyelids are very heavy or their vision is blurred.
A corneal dystrophy is a condition in which one or more parts of the cornea lose their normal clarity due to a buildup of material that clouds the cornea. These diseases:
Are usually inherited
Affect both eyes
Progress gradually
Don’t affect other parts of the body, and aren’t related to diseases affecting other parts of the eye or body
Happen in otherwise healthy people.
Corneal dystrophies affect vision in different ways. Some cause severe visual impairment, while a few cause no vision problems and are only discovered during a routine eye exam. Other dystrophies may cause repeated episodes of pain without leading to permanent vision loss. Some of the most common corneal dystrophies include keratoconus, Fuchs’ dystrophy, lattice dystrophy, and map-dot-fingerprint dystrophy.
Fuchs’ Dystrophy
Fuchs’ dystrophy is a slowly progressing disease that usually affects both eyes and is slightly more common in women than in men. It can cause your vision to gradually worsen over many years, but most people with Fuchs’ dystrophy won’t notice vision problems until they reach their 50s or 60s.
Fuchs’ dystrophy is caused by the gradual deterioration of cells in the corneal endothelium; the causes aren’t well understood. Normally, these endothelial cells maintain a healthy balance of fluids within the cornea. Healthy endothelial cells prevent the cornea from swelling and keep the cornea clear. In Fuchs’ dystrophy, the endothelial cells slowly die off and cause fluid buildup and swelling within the cornea. The cornea thickens and vision becomes blurred.
As the disease progresses, Fuchs’ dystrophy symptoms usually affect both eyes and include:
Glare, which affects vision in low light
Blurred vision that occurs in the morning after waking and gradually improves during the day
Distorted vision, sensitivity to light, difficulty seeing at night, and seeing halos around light at night
Painful, tiny blisters on the surface of the cornea
A cloudy or hazy looking cornea
The first step in treating Fuchs’ dystrophy is to reduce the swelling with drops, ointments, or soft contact lenses. If you have severe disease, your eye care professional may suggest a DMEK or DSAEK procedure to restore corneal clarity.
Keratoconus
Kerataconus is a progressive thinning of the cornea that distorts the corneal surface. The result is blurry vision from irregular astigmatism. It is the most common corneal dystrophy in the U.S., affecting one in every 2,000 Americans. It is most prevalent in teenagers and adults in their 20s.
Keratoconus causes the middle of the cornea to thin, bulge outward, and form a rounded cone shape. This abnormal curvature of the cornea can cause double or blurred vision, nearsightedness, astigmatism, and increased sensitivity to light.
The causes of keratoconus aren’t known, but research indicates it is most likely caused by a combination of genetic susceptibility along with environmental and hormonal influences. About 7 percent of those with the condition have a history of kerataconus in their family. Keratoconus is diagnosed with a slit-lamp exam. Your eye care professional will also measure the curvature of your cornea.
Keratoconus usually affects both eyes. At first, the condition is corrected with glasses or soft contact lenses. As the disease progresses, you may need specially fitted contact lenses to correct the distortion of the cornea and provide better vision.
In most cases, the cornea stabilizes after a few years without causing severe vision problems. A small number of people with keratoconus may develop severe corneal scarring or become unable to tolerate a contact lens. For these people, a corneal transplant may become necessary.
Lattice Dystrophy
Lattice dystrophy gets its name from a characteristic lattice-like pattern of deposits in the stroma layer of the cornea. The deposits are made of amyloid, an abnormal protein fiber. Over time, the deposits increase and the lattice lines grow opaque, take over more of the stroma, and gradually converge to impair vision.
Although lattice dystrophy can occur at any time in life, it most commonly begins in childhood between the ages of 2 and 7. In some people, amyloid deposits can accumulate under the epithelium of the cornea. This can erode the epithelium, and cause a condition known as recurrent epithelial erosion. This erosion alters the cornea’s normal curvature and causes temporary vision problems. It can also expose the nerves that line the cornea and cause severe pain.
To ease this pain, your cornea specialist may prescribe eye drops and ointments to reduce the friction of the eyelid against the cornea. In some cases, an eye patch may be used to immobilize the eyelid. The erosions usually heal within days, although you may have some pain for the next six to eight weeks.
By age 40, some people with lattice dystrophy have scarring under the epithelium that can impact vision to such an extent that the most effective treatment will be a corneal transplant. Although the early results of corneal transplantation are typically good, lattice dystrophy may reappear later and require long-term treatment.
Anterior Basement Membrane Degeneration
Anterior Basement Membrane Degeneration, also known as Map-Dot-Fingerprint Dystrophy, occurs when the basement membrane develops abnormally and forms folds in the tissue. The folds create gray shapes that look like continents on a map. There also may be clusters of opaque dots underneath or close to the maplike patches. Less frequently, the folds form concentric lines in the central cornea that resemble small fingerprints.
Symptoms include blurred vision, pain in the morning that lessens during the day, sensitivity to light, excessive tearing, and a feeling that there’s something in the eye.
Anterior Basement Membrane Degeneration usually occurs in both eyes and affects adults between the ages of 40 and 70, although it can develop earlier in life. Typically, Anterior Basement Membrane Degeneration will flare up now and then over the course of several years and then go away, without vision loss.
Some people can have Anterior Basement Membrane Degeneration but not experience any symptoms. Others with the disease will develop recurring epithelial erosions, in which the epithelium’s outermost layer rises slightly, exposing a small gap between the outermost layer and the rest of the cornea. These erosions alter the cornea’s normal curvature and cause blurred vision. They may also expose the nerve endings that line the tissue, resulting in moderate to severe pain over several days.
The discomfort of epithelial erosions can be managed with topical lubricating eye drops and ointments. If drops or ointments don’t relieve the pain and discomfort, there are outpatient surgeries including:
Anterior corneal puncture, which help the cells adhere better to the tissue
Corneal scraping to remove eroded areas of the cornea and allow healthy tissue to regrow
Laser surgery to remove surface irregularities on the cornea
Shingles is a reactivation of the varicella-zoster virus, the same virus that causes chickenpox. If you have had chickenpox, the virus can live on within your nerve cells for years after the sores have gone away. In some people, the varicella-zoster virus reactivates later in life, travels through the nerve fibers, and emerges in the cornea. If this happens, your eye care professional may prescribe oral anti-viral treatment to reduce the risk of inflammation and scarring in the cornea. Shingles can also cause decreased sensitivity in the cornea.
Corneal problems may arise months after the shingles are gone from the rest of the body. If you experience shingles in your eye, or nose, or on your face, it’s important to have your eyes examined several months after the shingles have cleared.
Iridocorneal endothelial syndrome (ICE) is more common in women and usually develops between ages 30-50. ICE has three main features:
Visible changes in the iris, the colored part of the eye
Swelling of the cornea
Glaucoma
ICE is usually present in only one eye. It is caused by the movement of endothelial cells from the cornea to the iris. This loss of cells from the cornea leads to corneal swelling and distortion of the iris and pupil. This cell movement also blocks the fluid outflow channels of the eye, which causes glaucoma.
There is no treatment to stop the progression of ICE, but the glaucoma is treatable. If the cornea becomes so swollen that vision is significantly impaired, a corneal transplant may be necessary.
Keratitis is an inflammation of the cornea. Noninfectious keratitis can be caused by a minor injury, or from wearing contact lenses too long. Infection is the most common cause of keratitis. Infectious keratitis can be caused by bacteria, viruses, fungi or parasites. Often, these infections are also related to contact lens wear, especially improper cleaning of contact lenses or overuse of old contact lenses that should be discarded. Minor corneal infections are usually treated with antibacterial eye drops. If the problem is severe, it may require more intensive antibiotic or antifungal treatment to eliminate the infection, as well as steroid eye drops to reduce inflammation.
Herpes of the eye, or ocular herpes, is a recurrent viral infection that is caused by the herpes simplex virus (HSV-1). This is the same virus that causes cold sores. Ocular herpes can also be caused by the sexually transmitted herpes simplex virus (HSV-2) that causes genital herpes.
Ocular herpes can produce sores on the eyelid or surface of the cornea and over time the inflammation may spread deeper into the cornea and eye, and develop into a more severe infection called stromal keratitis. There is no cure for ocular herpes, but it can be controlled with antiviral drugs.
A pterygium is a pinkish, triangular tissue growth on the cornea. Some pterygia (plural for pyterygium) grow slowly throughout a lifetime, while others stop growing. A pterygium rarely grows so large that it covers the pupil of the eye.
Pterygia are more common in sunny climates and in adults 20-40 years of age. It’s unclear what causes pterygia. However, since people who develop pterygia usually have spent significant time outdoors, researchers believe chronic exposure to UV light from the sun may be a factor.
To protect yourself from developing pterygia, wear sunglasses, or a wide-brimmed hat in places where the sunlight is strong. If you have one or more pterygia, lubricating eye drops may be recommended to reduce redness and soothe irritation.
Because a pterygium is visible, some people might want to have it removed for cosmetic reasons. However, unless it affects vision, surgery to remove a pterygium is not recommended. Even if it is surgically removed, a pterygium may grow back, particularly if removed before age 40.
Stevens-Johnson Syndrome (SJS), also called erythema multiforme major, is a disorder of the skin that also affects the eyes. SJS is characterized by painful blisters on the skin and the mucous membranes of the mouth, throat, genitals, and eyelids.
Often, SJS begins with flu-like symptoms, followed by a painful red or purplish rash of blisters that spread. SJS can cause severe conjunctivitis, iritis (an inflammation inside the eye), corneal blisters and erosions, and corneal holes. In some cases, SJS can lead to significant vision loss.
The most commonly cited cause of SJS is an allergic reaction to a drug or medication, particularly sulfa drugs. It is also associated with viral infections.
Treatment for the eye may include artificial tears or lubricating eye drops, antibiotics, or corticosteroids. About one third of those who develop SJS will have one or more episodes of the disease. SJS occurs twice as often in men as in women, and most often affects children and young adults under 30, although it can develop at any age.
A corneal abrasion is a scratch, scrape on the surface of your cornea. Fingernails, makeup brushes and tree branches are common culprits of corneal abrasions. Some other causes of corneal abrasion are rubbing your eye and having very dry eyes.
Corneal Abrasion Symptoms
- The feeling that something is stuck in your eye
- Red, painful, watery eyes
- Blurry or hazy vision
- Being extra sensitive to light
Why Do Corneal Abrasions and Corneal Erosions Hurt So Much?
The cornea has many nerve cells. Cells called pain receptors transmit pain to tell us about possible damage to the eye’s surface. In fact, there are hundreds of times more pain receptors in our cornea than there are in our skin.
Source: American Academy of Ophthalmology | Eye Smart
Corneal erosion is when the layer of cells on the surface of the cornea, called epithelium, loosens from the layer underneath. This is painful and makes your vision blurry or hazy.
Corneal Erosion Symptoms
Corneal erosion pain may start suddenly, often when you first wake in the morning. Your eyes get dry while you sleep, and your eyelid might stick to the cornea. If the epithelium is not firmly attached, opening your eyelids might peel the epithelium off.
Who Is at Risk for Corneal Erosion?
You are more likely to have corneal erosion if you:
- have very dry eyes
- have eyelids that do not close completely when you sleep
- had a corneal abrasion or injury to the cornea
- have a corneal disease (like corneal dystrophy)
- wear contact lenses that are not fitted properly
- wear contact lenses that have not been cared for properly
Source: American Academy of Ophthalmology | Eye Smart
Treatment Options
What is Laser Vision Correction?
Laser vision correction, which includes Custom LASIK and PRK, represents the most precise method to eliminate one’s glasses or contact lens prescription. Laser Vision Correction is a surgical technique that uses UV light and laser technology to reshape and restore the cornea. It has been used to treat recurrent erosions and corneal dystrophies and helps delay or postpone corneal grafting or replacement. Our specialists are the only Cornea-Fellowship-Trained doctors in Berks County and the most experienced with Bladeless LASIK. All laser vision correction procedures are performed in the safety and comfort of our on-site laser suite in our fully-licensed surgery center.
Corneas are the most commonly transplanted tissue worldwide. When a cornea is damaged, a cornea transplant can be used to restore a normal cornea. Corneal transplant surgery removes the damaged portion of the cornea and replaces it with healthy donor tissue. Multiple layers of cornea transplants exist and all are offered at Eye Consultants of Pennsylvania. Depending on each patient’s condition (most patients receiving a cornea transplant typically have corneas scarred from infection or trauma, but keratoconus is a common diagnosis as well), our corneal specialists will recommend a specific type of corneal transplant, either a partial or full transplant.
Currently, five different transplants exist, and all are offered at Eye Consultants of Pennsylvania. Two types are full thickness, and three are partial thickness:
DMEK and DSAEK are two similar partial thickness cornea transplants that treat patients with corneal edema (swelling) by replacing the cells on the inner layer of the cornea endothelium. This elegant, small incision procedure often allows improved vision in just weeks. Candidates for this procedure typically have Fuchs Dystrophy or a history of previous eye surgery.
DALK (Deep Anterior Lamellar Keratoplasty) is a partial thickness cornea transplant that treats patients with irregular corneas by replacing the cells on the outer layers of the cornea. This procedure typically has a 6-month to 1-year visual recovery. Candidates often have keratoconus or scars caused by previous infection.
PKP (Penetrating Keratoplasty) is a full thickness cornea transplant that treats severe corneal disease by replacing all layers of the cornea. It may take up to a year to see well after the procedure. Candidates often have severe keratoconus or previous corneal procedures.
The Boston Type 1 Keratoprosthesis (KPRO) is a full thickness artificial cornea transplant that treats severe corneal disease by replacing all layers of the cornea. This is an option in eyes that are not candidates for a conventional PKP.
Did you know that your eyes could help bring sight to someone after you die?
You can choose to donate your eyes to science and medicine. That donation may provide the gift of sight to someone who needs new corneas. Or you may help millions of people who benefit from research on other parts of the eye.
The cornea is the most commonly used donated eye tissue. Cornea transplants are performed to give vision back to people with corneal injuries or keratoconus.
The rest of the eye is just as important as the cornea in saving sight. Scientists working to find treatments and cures for eye disorders and diseases rely on donated tissue from the retina, lens and other parts of the eye. Researchers need donated eye tissue to help them develop new treatments and cures for cataracts, diabetic eye disease, glaucoma, macular degeneration and many other conditions.
Anyone Can Choose to Be an Eye Donor
Anyone can decide they want to donate their eyes for science and medicine. At the time of death, medical professionals will determine if your eye tissue can be used for transplants or research.
Some people wonder if their religion allows organ, eye and tissue donation. Rest assured that most faiths see it as a gift of charity. Check with your minister, pastor, rabbi, imam or other religious leader if you have questions.
It’s Easy to Become an Eye Donor
Tell your family you want to be an eye donor. Eye banks—the agencies that help get eye donations to medical and research institutions—will always ask your family if you told them you wanted to donate your organs.
In many states, you can sign a card at the driver's license bureau stating that you want to be an organ donor. You may say whether you wish to donate your eyes, organs or other tissues.
Choosing to be an eye donor is a special gift. You can be proud to know that you will help improve the quality of life for someone with little to no sight.
Here are links to websites where you can learn more about eye and tissue donation and find help in your area:
- United States Health Resources and Services Administration (USHRSA): organ donation and transplant information
- U.S. Department of Health and Human Services: OrganDonor.gov
- Donate Life America: DonateLife.net
Source: American Academy of Ophthalmology | Eye Smart
Does my insurance plan
cover my eye care?
Find out what insurance we accept and what is covered by insurance.
Learn more about our corneal eye care specialists
Physician information including education, training, practice location and more.
Schedule an Appointment
Schedule an appointment with one of our specialists.






